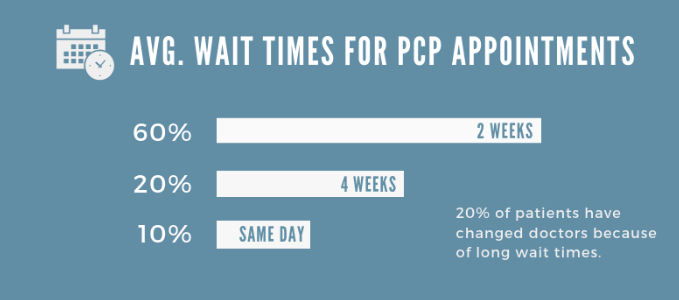
Have you called to schedule an appointment with your doctor lately? If so, how soon did they get you on the schedule? I'm guessing it wasn't the same day you called. In fact, only 1 out 10 folks are lucky enough to score a same day appointment.
80% of patients report having to wait 2 weeks or longer, just to see their primary care doc.
For primary care physicians, patients wait, on average, 18 minutes just to see the doc for 10 minutes when they are called in the room.
According to Vital’s Annual Report, 20% of patients have changed doctors due to long wait times and 30% have walked out of an appointment because of a long wait.
Imagine if you didn't have a PCP and had to schedule a new patient visit. These wait times can be even longer.
A 2022 survey from WSHA indicates that it now takes an average of 26 days to schedule a new patient physician appointment in 15 of the largest cities in the United States, up from 24.1 days in 2017 and up from 21 days in 2004.
According to the 2022 Primary Care Collaborative (PCC) Evidence Report the percentage of Americans with an ongoing primary care relationship has been declining, falling 10% between 2000-2019, from 84% to 74%.
Over 100 million Americans - nearly one-third of the nation - do not have access to a usual source of primary care due to a shortage of providers in their local community.
Projections suggest that by 2034 the shortages of primary care physicians will be between 17,800 and 48,000.
Houston, we have a healthcare problem.
The good news is that Direct Primary Care can alleviate these headaches. With most patients being seen same day and for no out of pocket expense, your health plan can eliminate these challenges for your staff.
These are challenges that our healthcare system needs to address for certain, but I would suggest that we don't sit around and wait for them to work themselves out. The aforementioned issues only scratch the surface of what is going wrong, in order to understand the value of DPC you must know what is really going on behind the scenes with PCPs in the fee for service model.
Enter stage left, the RVU.
Oh great, another health insurance / health care acronym. This is a pretty easy one to wrap your head around, RVU stands for relative value unit and this differ procedure to procedure.
Eric Bricker, MD does a great job of explaining how these work in this video:
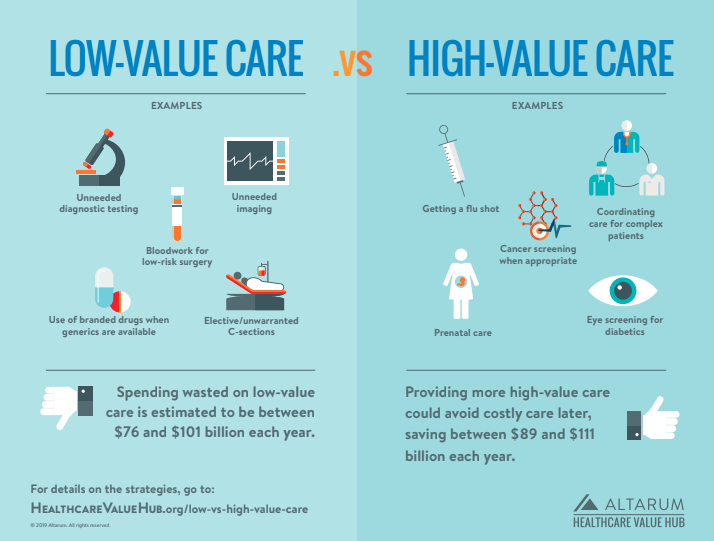
But don't stop there, there is a dirty little secret in how doctors are compensated that leads them to over prescribe low value care, just take a look at the chart below and see if you notice anything relative to your last physician visit.
In this video Dr. Bricker paints a picture of the pitfalls of RVUs as a measure of compensation:
So what is the alternative to the long wait times, lack of personalized care, and misaligned incentives in our healthcare system....
You guessed it, a Direct Primary Care Doctor is the best alternative. As opposed to a fee for service these doctors are paid a PEPM fee and your employees can visit that doctor as frequently as they would like, with no out of pocket expense.
The DPC provider typically offers same day or next day appointments. The in-office visit usually lasts from thirty to sixty minutes. The expanded access to the provider is possible because the average number of patients for a DPC practice can be less than half that of the traditional PCP model practice.
But let's not stop here, let's look at a cost comparison of this family of 5 and the routine care that they received over the course of a year.
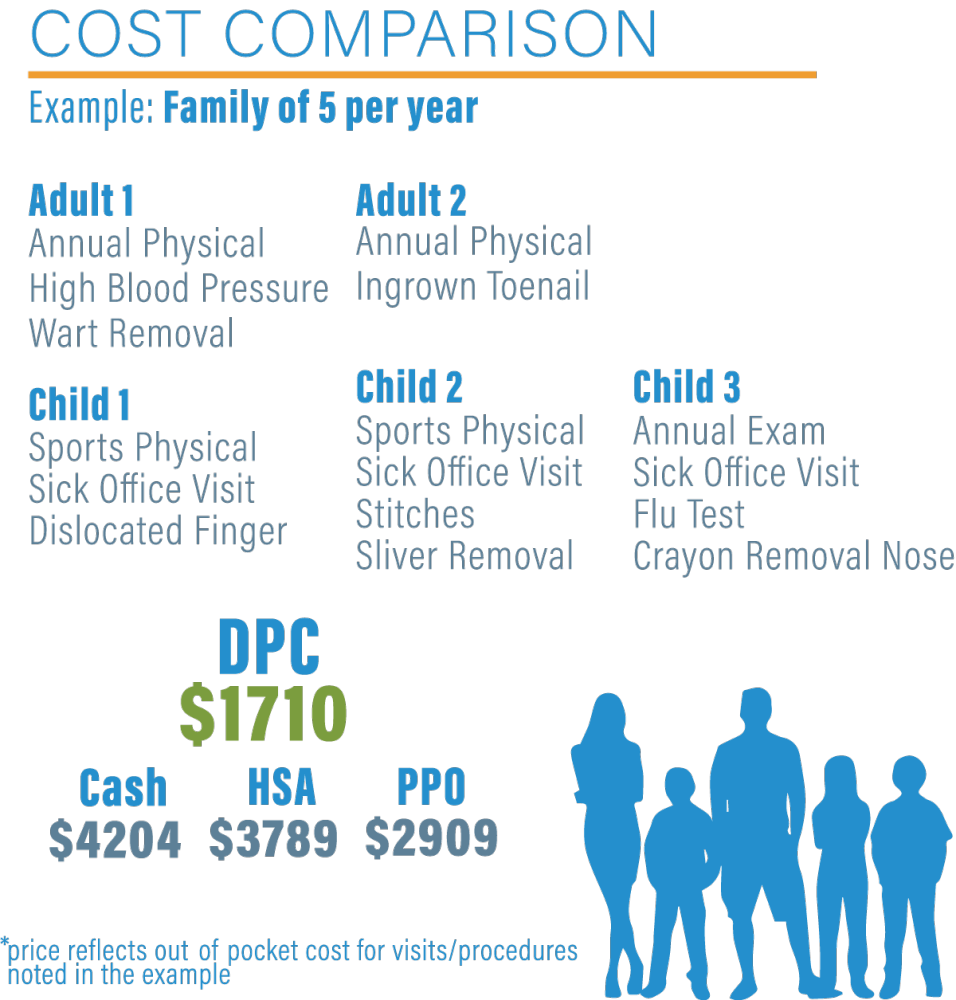
The goal of DPC is to provide patients with comprehensive, personalized care that is focused on prevention and early intervention, rather than just treating illnesses and symptoms after they occur.
Not to mention, DPC practices often have lower administrative costs than traditional fee-for-service practices, as they do not need to bill insurance companies for every service they provide.
All of this works in an employers favor to lower the cost of healthcare that your insurance plan has to cover.
DPC can help reduce healthcare costs in several ways:
- By focusing on prevention and early intervention, DPC can help patients avoid costly medical procedures and hospitalizations.
- DPC can help reduce the overall cost of healthcare by reducing the number of unnecessary tests, procedures, and medications.
- DPC practices can negotiate lower prices for medications and medical supplies, which can help reduce costs for patients.
- By eliminating the need for insurance billing, DPC practices can reduce administrative costs and pass those savings on to patients.
- DPC can also help reduce healthcare costs by improving patient outcomes and reducing the overall burden of chronic disease.
Here are some additional resources for you to learn more about how DPC can work for you on a local or national level:
Check out this savings analysis from one of our DPC Partners in the St. Louis market:
Savings analysis when DPC is integrated
Look at this brief on DPC from our national DPC partner Hint Health




